FOR HCPs
The STRIDE Clinical Trial:
A HEAD-TO-HEAD STUDY
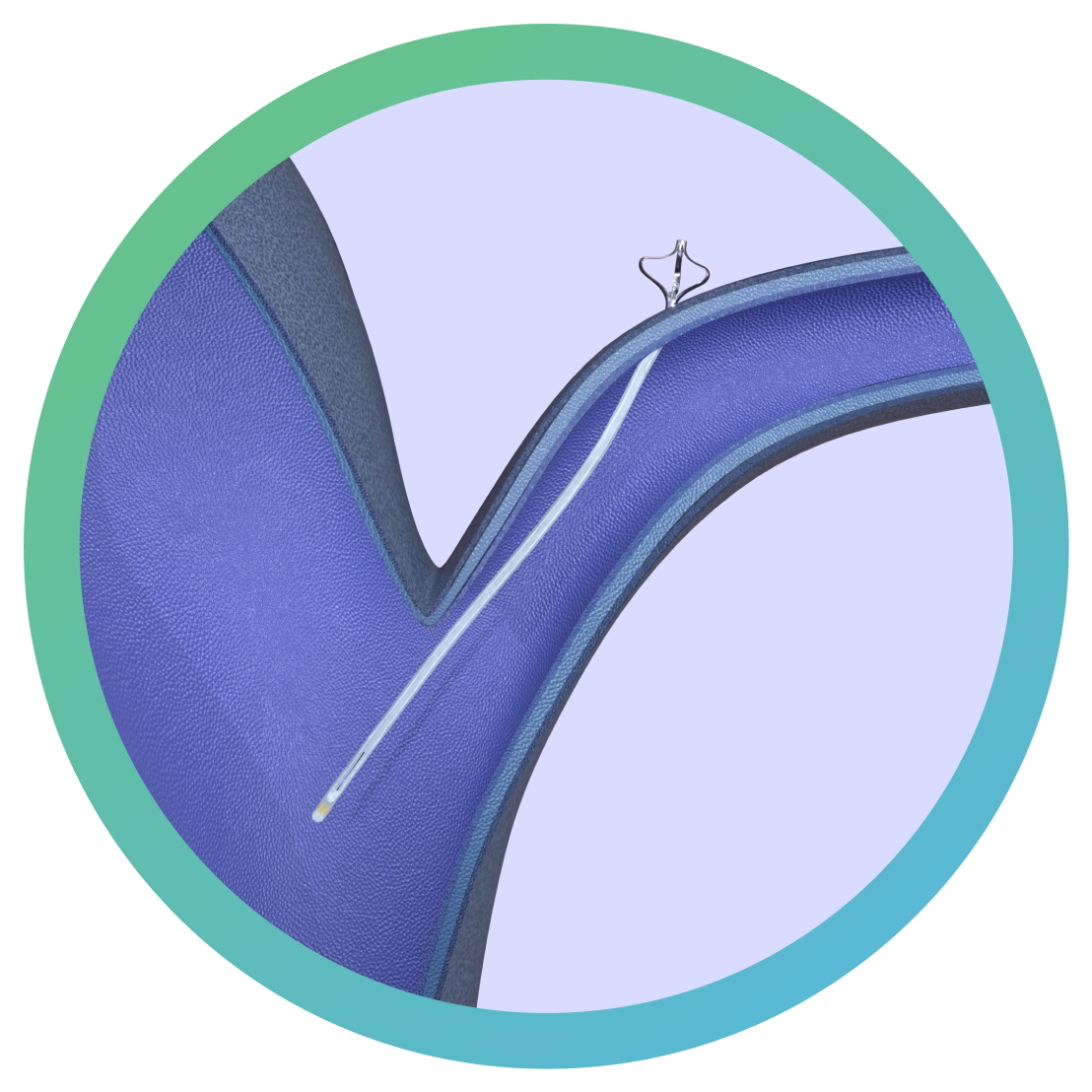
COMPARING THE eShunt®
SYSTEM AND VP SHUNTS
The STRIDE Clinical Trial:
A HEAD-TO-HEAD STUDY COMPARING THE eShunt® SYSTEM AND VP SHUNTS
The STRIDE clinical trial is evaluating the safety and efficacy of the investigational eShunt® System—an endovascular approach to normal pressure hydrocephalus (NPH) treatment.
Caution: The eShunt® System is an investigational device. Limited by United States law to investigational use only. The safety and effectiveness of the eShunt® System have not been established.
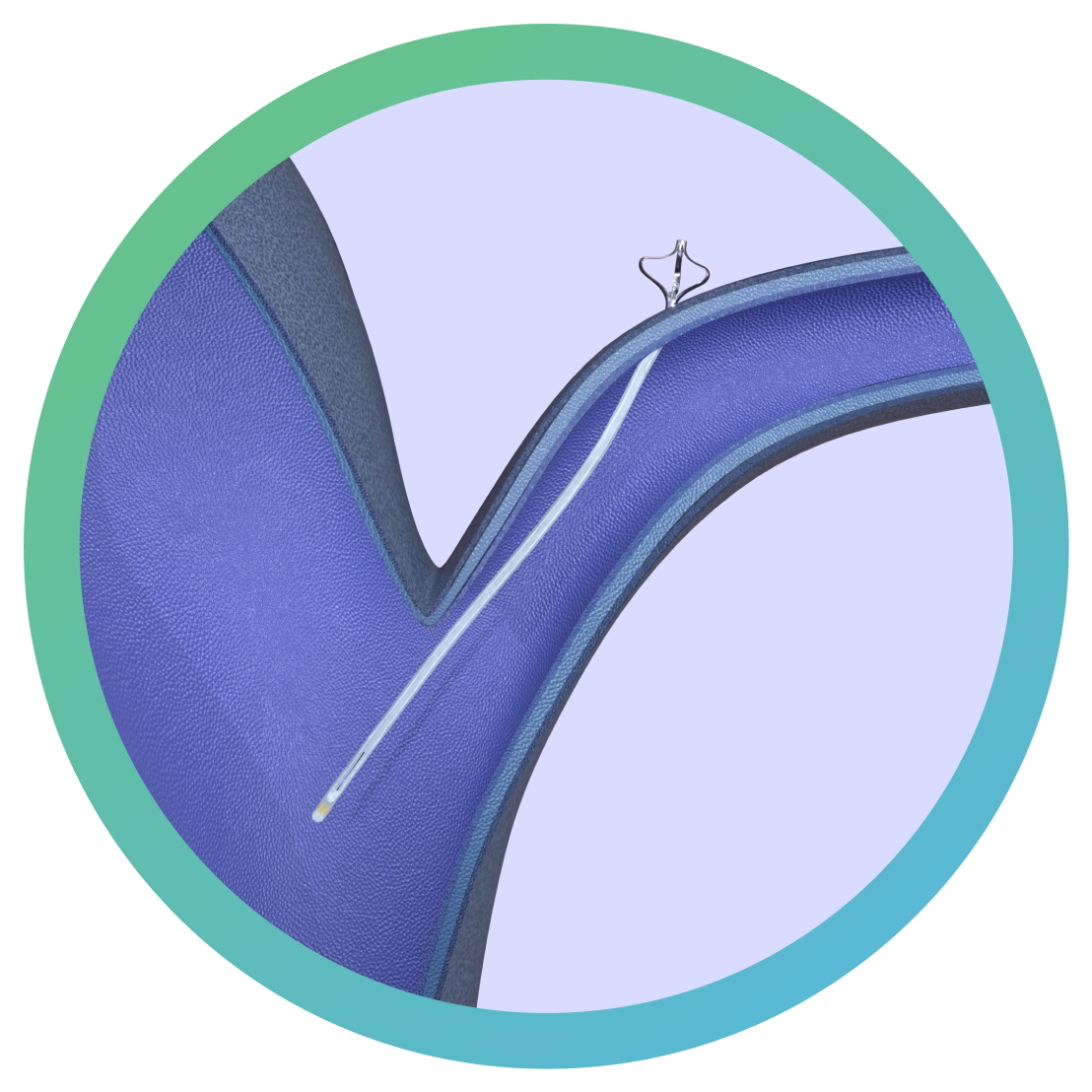
The STRIDE clinical trial is evaluating the safety and efficacy of the investigational eShunt® System—an endovascular approach to normal pressure hydrocephalus (NPH) treatment.
Caution: The eShunt® System is an investigational device. Limited by United States law to investigational use only. The safety and effectiveness of the eShunt® System have not been established.